Building Healthier Schools: Cone Health’s Telehealth Approach

The Challenge of School-Based Healthcare
In many schools across the United States, chronic absenteeism is a critical barrier to education. This is particularly true for schools with Title I status. During the peak of the COVID-19 pandemic in 2022, a staggering one-third of students in such schools were chronically absent—a situation that failed to improve even as the pandemic waned in 2023. At the heart of this issue was a glaring lack of accessible healthcare solutions, which contributed to significant academic disruption and increased health-related burdens on families.
The Conflict in Schools
Before the introduction of telehealth programs, schools struggled not only with high rates of absenteeism, but also with integrating effective healthcare solutions that did not interrupt educational delivery. The traditional model of school-based healthcare failed to meet the needs of students and educators alike, causing health issues to become educational impediments.
A Revolutionary Transformation: Cone Health’s Telehealth Program
Dr. John Jenkins, Executive Medical Director of School-Based Care at Cone Health, spearheaded a transformative approach to tackle these persistent challenges. Cone Health introduced the Whole School, Whole Community, Whole Child model, which serves as a healthcare initiative and a strategic educational partnership.
The program was designed with the intention to ensure equitable access to healthcare. It is aimed at returning students to the classroom by addressing and reducing the impact of illness. Here’s a closer look at the strategic partnerships essential to the program’s success:
Strategic Partnerships and Collaborations
- School District Partnerships
- From day one, the initiative was built as a partnership with the school district.
- A shared vision was maintained with the superintendent and the school board, focused on measuring educational factors such as absenteeism, early dismissals, academic progress, and behavioral issues.
- Dyad partnerships were established with the Chief of Student Services, Director of Student Health, and Director of School Nursing.
- The relationships, roles, and outcome expectations were formalized in a memorandum of understanding to ensure clarity and accountability.
- County Government and Public Health Collaborations
- The program emphasized collaboration over competition, encouraging research into state mandates for school health and nursing.
- It verified whether the state had a delegated service model and if the CDC’s Whole School, Whole Community, Whole Child (WSCC) model was enacted.
- Another memorandum of understanding was established, covering both PHI (HIPAA) and PII (FERPA), to co-develop pathways for student encounters and set up a regular cadence of meetings with clinical stakeholders.
- The program’s telepresenters did not replace school nurses, but rather enhanced the WSCC model through delegated partnerships.
- Healthcare Partnerships
- Decisions were made on the model for provider delivery, including dedicated urgent care Advanced Practice Providers, system partnerships with hospital practices, and community partnerships with independent and safety net practices.
- The program aimed to promote reliable care through standard work and pathways for telepresenters, including considering charging for services.
- Important internal partnerships were reinforced with school nurses, social workers, guidance counselors, and behavioral health services staff to provide comprehensive care and address social determinants of health.
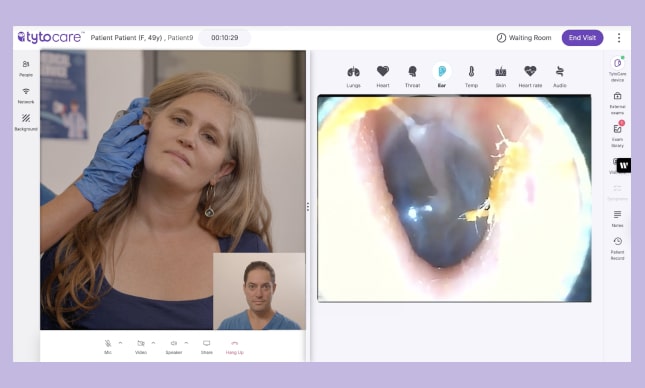
Learn from the Summit
This innovative program at Cone Health has set a benchmark for integrating telehealth into school settings, demonstrating significant improvements in student attendance and health outcomes. To learn more about creating successful school health programs through intentional design and strategic partnerships, watch the full School Health Virtual Summit on TytoCare’s webinar platform.