
Innovating Product Design for Growth and Member Engagement








- Product Strategy: Discussion on timing, market fit, and customer feedback and validation.
- Plan and Product Design: Focus on designing benefits that matter, affordability, accessibility, and niche products.
- Member Activation and Engagement: Exploration of strategies to drive meaningful engagement and improve member feedback loops.
Product design in healthcare must balance innovation with market needs, emphasizing timing, product-market fit, and customer feedback
We tend to over index on three things: timing, product-market fit, and customer feedback and validation.

Roni Mansur
Tailored and niche products can significantly improve member engagement and satisfaction by addressing specific needs and preferences
Instead of just giving everybody everything, our philosophy is to design benefits that really matter.

Lena Perelman
Integrated and holistic benefit design, driven by clinical insights, can enhance member outcomes and reduce costs
We’re working on bidirectional data sharing to ensure that clinical programs refer to each other smoothly.

Maria Baker
Continuous feedback and iterative improvement are crucial for the success of new healthcare products
Solutions that are not only high value and high convenience to the consumer, but also good for the provider partner, and that they enable them to practice more effectively and a higher level of quality in that virtual setting, are where we see the strongest adoption.

Suzi Pigg
Learn more
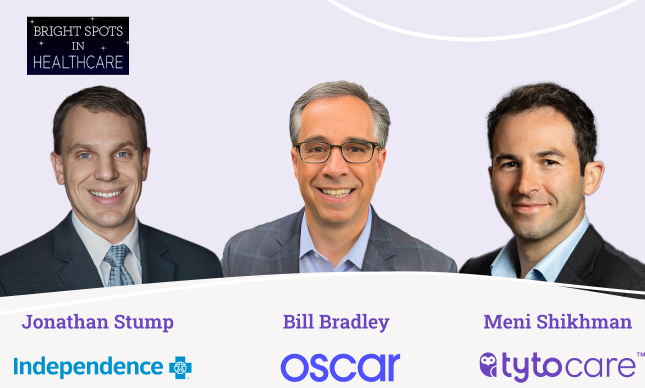
Differentiating Your Product and Benefit Design to Drive Enrollment
In this webinar, we explored practical insights and actionable strategies on how health plans can leverage various solutions effectively to optimize pricing structures; and explored technology adoption, cost-effectiveness, and market competitiveness. The panel of industry experts shared experiences and real world examples; highlighting successful implementations of solutions that have positively impacted pricing strategies. Hear from:

Behavioral Science: Increasing Member Engagement in your Digital Offering
Healthcare insurers are increasingly moving to virtual-first and hybrid offerings. For these programs to succeed, member adoption will be important. Join Richard Mathera, Managing Director at Irrational Labs, and Hagai Heshes, Head of Product Marketing at TytoCare, as they discuss the role of behavioral design in creating digital solutions with high adoption and engagement rates […]
